Cervical cancer is central to the emerging cancer pandemic in low- and middle-income countries. This malignancy is caused by a chronic infection of selected types of the human papilloma virus (HPV). In 2008 cervical cancer was the fourth leading cause of cancer death in women worldwide, and the leading cause of cancer death in Africa and Southeast Asia. The number of lives lost to this preventable disease is a global failure of the largest scale if one considers that the health system in western and high income countries have developed very efficient programmes to prevent, detect, and treat cervical cancer which, in fact, have reduced disease incidence and mortality. In 2008, cervical cancer caused an estimated 275,100 deaths globally. Ninety percent of these deaths occurred in developing parts of the world, where access to screening and treatment are often non-existent and adolescent girls are not receiving vaccination for HPV. The HPV vaccine represents a major tool for primary prevention of the disease as it can prevent up to 70 percent of cervical cancer cases. Moreover, cost-effective procedures are now available to detect and treat cervical pre-cancer thus promoting secondary prevention. We ought to promote public awareness about cervical cancer in African countries, educate health professionals, and improve access to screening. Issues that are critical to cervical cancer screening are public awareness (by women and local general practitioners), diagnostic capacity (in terms of availability of properly trained people in cytology and gynaecologists capable of managing cervical cancer and precancer), updating treatment modalities and outlets, the network of referral centres, and HIV coinfection.
Talking about preventable cancer in African women: facts, thoughts, questions, beliefs, related topics and strategies to fight against cancer of the uterine cervix and the breast.

lunedì 12 settembre 2011
sabato 30 luglio 2011
male circumcision to prevent HIV and HPV infections
Male circumcision, i.e. the surgical removal of some or all of the foreskin (or prepuce) from the penis, has been associated with a lower risk for HIV infection in international observational studies and in three randomized controlled clinical trials. How can it be explained? Compared with the dry external skin surface, the inner mucosa of the foreskin is thinner than other penile skin, has a higher density of cells which are targets for HIV, and shows greater susceptibility to traumatic epithelial disruptions (tears) during intercourse, providing a portal of entry for pathogens, including HIV. In addition, the microenvironment in the preputial sac between the unretracted foreskin and the glans penis may be conducive to viral survival. Removal of prepuce from the penis causes a transformation of this mucosa which becomes thicker and less susceptible to trauma and infection. It has been shown that male circumcision could reduce male-to-female transmission of HIV, although probably to a lesser extent than female-to-male transmission. Although links between circumcision, culture, religion, and risk behavior may account for some of the differences in HIV infection prevalence, the countries in Africa and Asia with prevalence of male circumcision of less than 20% have HIV infection prevalences several times higher than those in countries in these regions where more than 80% of men are circumcised. Lack of male circumcision has also been associated with sexually transmitted genital ulcer disease and chlamydia, infant urinary tract infections, penile cancer, and cervical cancer in female partners of uncircumcised men. The latter two conditions are related to human papillomavirus (HPV) infection. Male circumcision may represent an effective additional procedure to primarily prevent cervical cancer in women living in African countries, the other being safe sex, vaccination of females and males against HPV.
Diversi studi scientifici hanno dimostrato che la circoncisione nel maschio, cioè la rimozione del prepuzio dal pene, si associa ad una diminuzione del rischio di infezione da HIV. Quale ne è il motivo? In effetti, la mucosa del pene che sta all’interno del prepuzio è più sottile della cute esterna del prepuzio stesso, contiene una quantità superiore di cellule che sono il bersaglio del virus HIV ed, essendo più delicata, risulta più suscettibile a microtraumi. Infine il microambiente del sacco prepuziale favorisce la concentrazione del virus. Se invece si rimuove la porzione retraibile di cute e mucosa che riveste il sacco prepuziale, la mucosa sottostante si trasforma diventando più spessa e più simile alla cute. Ciò riduce fortemente il rischio di contrarre l’infezione e di ritrasmetterla. A riprova di ciò è stato osservato che nei paesi in cui la circoncisione è praticata in meno del 20% della popolazione maschile, la prevalenza della malattia è di molto superiore a quella riscontrata nei paesi in cui la circoncisione è praticata in più dell’80% dei maschi. La mancanza di circoncisione favorisce inoltre l’incremento di altre malattie sessualmente trasmesse, come le ulcere genitali, le infezioni urinarie infantili, le infezioni da clamidia, il carcinoma del pene e il carcinoma della cervice uterina nelle partner degli uomini non circoncisi. Queste due forme di carcinoma sono dovute all’infezione da virus papilloma umano (HPV). La circoncisione maschile può rappresentare un ulteriore mezzo per favorire la prevenzione primaria del carcinoma della cervice uterina aggiungendosi alla modifica degli stili di vita e alla vaccinazione contro il virus sia delle femmine che dei maschi.
martedì 14 giugno 2011
countdown to zero cases of newborn HIV infections
A baby is born with HIV nearly every minute, almost all of them in sub-Saharan Africa. In 2009, an estimated 370,000 children were infected at birth with HIV, almost all in low- and middle-income countries. The United Nations (UN) and the United States (US) government have recently launched an initiative to eliminate HIV among babies by 2015 by treating HIV-positive pregnant women, cutting infection among their babies to less than 5%. The plan, called Countdown to Zero, was developed by a team led by UNAids and the US President's Emergency Plan for AIDS Relief. It will cost an estimated $2.5bn (£1.5bn) to care for 15 million women, double those currently being treated. A key element of the campaign is to ensure that all women, especially pregnant ones, have access to quality life-saving HIV prevention and treatment services for themselves and their children. Achieving the goal could be "the beginning of the end of the story, because that opens the prospect for an Aids-free generation," said Michel Kazatchkine, head of the Global Fund to Fight AIDS, Tuberculosis and Malaria."We are here today to ensure that all children are born healthy and free of disease. We are here to ensure that their mothers live to see them grow," UN Secretary General Ban Ki-moon said at the launch of the plan."We believe that by 2015 children everywhere can be born free of HIV and that their mothers can remain healthy," said Michel Sidibe, executive director of UNAids. Cutting the number of new cases of HIV infection will also play a major role in reducing the number of immunodepression-related cancers in the developing world. In women, it will result in the reduction of new cases of cancer of the uterine cervix as HIV and HPV coinfection represents a major risk for the tumor to develop and behave aggressively. An HIV-infection free generation is really a major goal for mankind.
Quasi ogni minuto nell’Africa sub sahariana nasce un bambino portatore di infezione da HIV acquisita per trasmissione materno-fetale. Si stima che nel 2009 ne siano nati 370000, la maggioranza di essi nei Paesi in via di sviluppo. I governi delle Nazioni Unite e degli Stati Uniti hanno recentemente lanciato l’iniziativa di ridurre per il 2015 l’incidenza di infezione neonatale da HIV al di sotto del 5%. Per fare ciò si tenterà di fornire alle donne Africane, in particolar modo quelle in gravidanza, l' accesso a cure efficaci dell'infezione con l’intento di trattare soprattutto i loro bambini. Questo programma denominato “cowntdown to zero” è stato concepito dalla UNAids e dal Piano di Emergenza anti-AIDS del Presidente degli Stati Uniti, dovrebbe interessare 15 milioni di donne e costerà 2.5 miliardi di dollari. Ottenere questo risultato potrebbe rappresentare l’inizio della fine dell’AIDS e la creazione della prima generazione Africana senza la malattia. La riduzione dell’incidenza dei nuovi casi di AIDS contribuirà inoltre ad abbattere l'incidenza dei tumori correlati all’immunodeficienza acquisita che colpiscono duramente le popolazioni dei paesi più poveri. Per ciò che riguarda le donne si potrà anche verificare la riduzione dei nuovi casi di carcinoma della cervice uterina in quanto questo tumore, dovuto all'infezione cronica da virus papilloma umano (HPV), si sviluppa con particolare frequenza nelle donne portatrici di infezione da HIV. In conclusione, la sconfitta dell’AIDS rappresenta un obiettivo primario per l’umanità intera.
mercoledì 18 maggio 2011
uterine cervical cancer in the population of Nosy Be, Madagascar
 |
| Pathologist at the microscope and local staff reviewing the cytological reports |
So far, we have examined cumulatively 278 women aged 16 to 57. In both missions we managed to perform pap smear evaluation with immediate reporting and immediate colposcopy and biopsy on a same-day basis. To summarize, pap smear sampling started early in the morning and was performed by two physicians, then slides were immediately stained and interpreted by a Pathologist who was able to release a cytopathological report at the end of the morning. Then, women bearing abnormalities in their pap smear were invited to undergo immediate colposcopy which was performed in the early afternoon. Biopsy samples were then collected and processed for histological evaluation. Histological processing was completed in Italy at the department of Pathology, Fatebenefratelli Hospital, in Milano, Italy.
 |
| women waiting for their turn for pap smear sampling |
Overall, we detected 5 women with high grade lesions according to the Bethesda System, 2001, and three of them were diagnosed as having squamous cell carcinoma in situ on biopsy examination. Low grade lesions were found in other 25 women who are going to be re-evaluated within 6 months after the first pap smear. The overall cumulative incidence of pap smear abnormalities in this population is 10.79%, and this value is higher than the World Health Organization’s estimates of 10% (see "Comprehensive Cervical Cancer Control. A guide to essential practice", p. 40, World Health Organization, 2006) for the previously unscreened population in Madagascar. The above value is about 5-fold to 8-fold higher than the incidence of abnormalities in the screened population living in countries of the high-income developed world.
In un precedente post ho parlato della missione medica da noi eseguita in settembre del 2010 e finalizzata a promuovere la prevenzione del carcinoma della cervice uterina nella popolazione residente di Nosy Be, in Madagascar. Tale missione è stata ripetuta in Aprile 2011 e ha avuto luogo presso il Dispensario della Organisation Medicale Interenterprises di Nosy Be (OMINO) a Hellville, il capoluogo dell'isola. I dati raccolti confermano la nostra precedente impressione che l’incidenza di questa neoplasia in quell’area geografica è decisamente elevata. Abbiamo esaminato in tutto 278 donne e identificato 5 casi con lesioni ad "alto rischio" di cui 3 con carcinoma. Sono state identificate inoltre 25 donne portatrici di lesioni a “basso rischio” che verranno sottoposte a controllo ravvicinato. In entrambe le missioni abbiamo provveduto a eseguire la lettura immediata del pap test allo scopo di poter sottoporre le pazienti che necessitavano di colposcopia e biopsia nello stesso giorno. Questa modalità operativa ha consentito di annullare la quota di casi che solitamente non si ripresenta al controllo quando le pazienti vengono riconvocate a distanza di tempo dal pap test e ciò ha ottimizzato gli effetti dello screening. L’incidenza di lesioni riscontrate, pari al 10,79%, appare decisamente elevata se si pensa che l’Organizzazione Mondiale della Sanità stima un’incidenza massima del 10% per la popolazione del Madagascar. L’incidenza è da 5 a 8 volte superiore a quella riscontrata nella popolazione femminile sottoposta a regolare screening nei paesi occidentali.
martedì 10 maggio 2011
Metronomic chemotherapy to treat cancer in low-resources countries
giovedì 5 maggio 2011
HPV vaccination in male to prevent uterine cervical cancer
The origin of cancer of the cervix uteri is directly linked to a chronic infection of selected (so called “high risk”) types of human papilloma virus (HPV). The virus is readily transmitted from men to women by the sexual intercourse and greatly affects the risk of disease in women. It is for this reason that understanding the nature of HPV in men is of crucial public health importance and can be used in modeling to establish whether vaccinating men against HPV would be cost effective. An Article published by Professor Anna R Giuliano and colleagues, of the H Lee Moffitt Cancer Center and Research Institute, Tampa, FL, USA, in the prestigous medical journal the Lancet shows that approximately 50% of men from a sample of the general population are infected with the virus. The study analysed 1159 men aged 18 to 70 years (mean 32 years) from the USA, Brazil, and Mexico, all of whom were HIV negative and had no history of cancer. They were assessed every six months for an average of more than two years. The incidence of a new genital HPV infection with any HPV type was 38.4 per 1000 person months. The chances of cancer-causing (oncogenic) HPV infection was 2.4 times higher from men who had had many female partners compared with no partners or just one partner. The authors say: 'We noted no association with age and incidence of any, oncogenic, or non-oncogenic HPV types, although the probability of clearing these infections increased with age." They conclude: "The incidence of genital HPV infection in men was high and relatively constant across age groups in Brazil, Mexico, and the USA. The results from this study provide much needed data about the incidence and clearance of HPV infection in men; these data are essential for the development of realistic cost-effectiveness models for male HPV vaccination internationally". HPV vaccination of men will protect not only them but will also have great implications for their sexual partner. Vaccination of both females and males could represent the best way to fight uterine cervical cancer.
domenica 24 aprile 2011
Education to breast health promotes early diagnosis of cancer
Women living in the developing countries have a higher probability of dying from breast cancer as compared to those of the high income western world. According to the Globocan/IARC data the number of deaths as a percentage of incident cases in 2008 was 48% in the former and 24% in the latter. Exactly twofold. Available evidence on stage at diagnosis indicate that a much higher proportion of cases in the developing world are detected in late stages thus the potential of survival is poorer. Many reasons are given to explain these data: the stigma of breast cancer and the associated societal implications of its treatments (especially mastectomy) discourage women from seeking care early on; lack of knowledge about breast health; scant options for early detection due to limited access to routine care and examinations; and lack of access to mammography and to affordable, high-quality treatment options. In summary, lack of education to breast health awareness and complex cultural barriers do play a significant role in delaying breast cancer detection in developing countries. Increased awareness of breast cancer symptoms and potential of successful treatment of the tumor in early stages would be of great help to improve survival even without widespread use of mammography, advanced surgical procedures, and adjuvant therapies. In fact, if we examine the reasons for the remarkable improvements in the probability of survival for women diagnosed with breast cancer in the USA as compared to 60 years ago it is possible to realize that a significant result had been achieved also prior to the introduction of massive screening of the tumor simply by means of education to improve breast health awareness and to breast self examination. In the low-income developing world, the provision of better education is bound to provide a solid foundation for reducing stigma and fear that will make more effective the introduction of complex technologies for early diagnosis and the use of highly expensive drugs for adjuvant therapy.
sabato 12 marzo 2011
too little benefit from regular mammogram in women in their 40s
Screening by routine mammogram is intended to catch breast cancer in women while it is still small and presumably easier to treat. So far, annual or biennial mammography has been advised to women starting from the age of 40. Some recently collected data have shown, however, that regular mammogram provides very modest benefit in terms of reducing death for breast cancer in women aged 40 to 49. In fact, without screening, 3.5 out of every 1,000 women in this age group will die of breast cancer in the next 10 years but regular mammography reduces that number to 3, i.e. the benefit derived from screening is only 0.5 per 1000 women!. Indeed, it has also been calculated that to save one life in this age group, 1,900 women must be screened annually for 10 years. The other 1,899 women will receive no benefit from mammography over that period, though they will field 1,330 call-backs for reassessment and 665 breast biopsies, and eight of them will be diagnosed with cancers whose prognosis will not be altered by detection via mammogram — either because they would never become dangerous or because they are so aggressive that there's little to be done. Data reported in recently published studies wherein women were randomly assigned to either a screening and a non screening group seem to confirm this contention. The U.S. Preventative Services Task Force thus decided in November 2009 that whether the benefits are worth the risks is a value judgment each woman should make for herself. Regular mammogram is instead highly reccomended after the age of 50 due to a significantly increased risk of breast cancer. In developing countries the incidence of breast cancer is significantly lower than in high income developed world but mortality due to the tumor is much higher. Even if the chance of detecting breast cancer in women younger than 50 is rather remote, the higher risk of dying of the disease may suggest that regular mammogram in women of developing countries in their 40s should still be encouraged .
sabato 5 marzo 2011
breast cancer and passive smoking
Smoking is associated with an increase in breast cancer risk among postmenopausal women but there seems to be a definite increase also in non smoker women who have been extensively exposed to second hand smoke. These data were recently reported in the British Medical Journal. The study was based on the observation of nearly 80,000 women aged between 50 and 79 years enrolled in the Women’s Health Initiative Observational Study from 1993 to 1998. Invasive breast cancer appeared in 3,250 women during 10 years of follow-up. Smokers had a 16% increased risk of developing breast cancer after the menopause as compared to non smokers. For ex-smokers the risk was 9% and continued for up to 20 years after an individual had stopped smoking. The highest breast cancer risk was found among women who had smoked for over 50 years or more. What about non smokers? women who had never smoked but had lived or worked with smokers for prolonged times also appeared to be at increased risk for breast cancer. In particular, over 10 years’ exposure in childhood, over 20 years’ exposure as an adult at home and over 10 years’ exposure as an adult at work, increased the risk by 32% compared with those who had never been exposed to passive smoking. In low income and developing countries large declines in mortality are projected to occur in the near future for all of the principal communicable disease, maternal, peri-natal and nutritional causes, with the exception of HIV/AIDS. Meanwhile, the aging of the global population will result in significant increases in the total number of deaths caused by most non-communicable diseases such as cancer. In particular, increases in the prevalence of tobacco consumption and significant lifestyle changes in the population are bound to produce an increased risk of breast cancer in African women. Thus, efficient screening procedures for early detection of the disease need urgently to be implemented.
martedì 1 marzo 2011
HPV vaccination and cervical cancer
Cervical cancer is the second most common cancer in women worldwide and it is linked to persistent infection by human papilloma virus (HPV). Vaccination against HPV represents an important tool to obtain a primary prevention of the tumor. There are many strains of the virus but only a small number of them causes cancer. An international team of researchers has recently identified eight strains of the HPV responsible for more than 90% of cervical cancer cases. The study, which was published in the prestigious medical journal The Lancet, examined 60 years of data from 10575 cases of invasive cervical cancer in 38 countries. HPV was found in about 85% of cancer samples. More than 90% of these cases were caused by HPV types 16, 18, 45, 33, 31, 51, 58 and 35, in descending order of frequency. Only 1% of cases worldwide were linked to the infection by HPV types 26, 30, 61, 67, 69, 82 and 91. The former group of eight strains will represent the target for the next generation of HPV vaccines. Currently two vaccines are available in the market, Cervarix and Gardasil, which cover the infection by HPV strains 16 and 18. Gardasil covers 11 additional non oncogenic HPV strains which are responsible for genital warts. Prophilactic efficacy of the two HPV vaccines is almost 100% and they can prevent cancer cases directly linked to infection by HPV strains 16 and 18. Efficacy of the vaccination is obviously dependent upon the recipient not having been already infected with that type of HPV. Cancer cases due to 16 and 18 HPV strains represent about 60%-70% of total cases. Future efforts will focus on the production of second generation vaccines covering in addition the other six HPV strains (45, 33, 31, 51, 58 and 35) in order to prevent more than 90% of cases.
lunedì 21 febbraio 2011
breast cancer risk factors and triggers
The genetic risk factors for breast cancer to develop are age, being a female, and having a family history of the tumor. In developed countries the risk of breast cancer in women at the age of 29, 39, and 49, is, respectively, one in 2000, one in 215, and one in 50. The lifetime risk of breast cancer reaches the highest values in women 70 and older: one in eight !. In the latter age group the incidence has progressively increased in the last fifteen years as it was one in ten in 1997 and one in nine in 2003. Why is it happening? Cancer is a genetic disease but it needs some triggers to develop. There is now a good evidence that triggers of breast cancer can be found in lifestyle and environment and most probably are the followings: having fewer children and in later life; reduced breastfeeding; widespread hormone replacement therapy (administered to contrast the debilitating symptoms of the menopause); increased alcohol consumption, and excess of weight (especially after menopause). Oestrogen and other hormones are strongly implicated in breast cancer, and both pregnancy and breastfeeding reduce the amount of circulating hormone. Each birth decreases the risk of breast cancer by 7%. Every year of breastfeeding cuts the risk by 4.3%.
Women in developing countries have lower rates of breast cancer mainly because they start to have babies at a much younger age and have higher parity. In Sub-Saharan Africa, higher incidence rates and relative frequencies of breast cancer have been reported in association with urban than with rural residence but, in any case, the incidence of the disease is much higher among white women in Africa than among black African women. Notice that this is just the opposite of what has been reported for afroamerican women as compared to white women in the USA (see my previous post on the topic). In the future decade a progressive change in women’s lifestyle (on the model of western women) will probably take place also in many countries of the African continent and this will parallel a rise in breast cancer incidence. We should get prepared: the fight against breast cancer can be successful only if local health systems provide early diagnosis and proper treatment facilities.
mercoledì 16 febbraio 2011
Village health workers’ role in primary prevention of diseases
 |
| plumeria (frangipani) |
Villagers in many developing countries rarely see doctors or nurses. In fact, a fraction of medical graduates and nurses of English speaking parts of Africa or southern Asia, often emigrate to wealthy countries (Canada, USA, UK and Australia) as they are attracted by better pay and working conditions. Those doctors who, instead, remain in their home country tend to stay in the cities and not in rural areas. Similarly, nurses are rarely tempted by rural villages. Doctors and nurses, however, are not necessary to improve rural health in developing countries. Two very successful programs in desperately poor parts of India’s Maharashtra State which were described in an interesting report appeared in the New York Times show that people with no or little formal medical training do successfully substitute for doctors and nurses. Once properly trained, these ordinary women and men help prevent most rural sickness by teaching people very simple acts such as the use of clean water, waste-disposal systems and more diverse farming. As a matter of fact, village health workers do have a huge impact on the health and prosperity of the community they serve. They visit pregnant women repeatedly, attend births, teach mothers about how to keep their babies healthy and check in on the children often. They teach new mothers how to feed and care for their babies and how to treat diarrhea and fever. Children get regular immunizations, and tuberculosis, scabies and leprosy are properly and effectively prevented. The main role of these health rural workers is teaching the community some essential preventive measures. Their potential role also in the prevention of HIV infection and cancer of the cervix uteri in young women should be properly and adequately stressed. They can really induce a major behavioral change in sex habits of the population by means of interpersonal communication activities. Health workers should be trained on this topic too and prevention of tumors should become a novel goal of these programs.
domenica 13 febbraio 2011
AIDS prevention in Zimbabwe
 |
| tropical nymphaea |
According to the United Nations, about 33.3 million people worldwide are infected with HIV and the majority of those live in sub-Saharan Africa. The virus can be controlled with cocktails of drugs, but there is no cure and nearly 30 million people have died of HIV-related causes since the disease first emerged in the 1980s. The good news is however that the disease has taken a dramatic downturn in Zimbabwe, a country where its incidence was among the highest in the world. In fact, people infected with HIV were 29% in 1997 but ten years later, in 2007, they were 16%. How was it possible? The answer is: primary prevention. Zimbabweans have primarily been motivated to change their sexual behavior because of increased awareness about AIDS deaths which heightened their fears of catching the human immunodeficiency virus that causes it. The behavioral changes associated with HIV reduction consisted mainly in reductions in extramarital, commercial, and casual sexual relations, and associated reductions in partner concurrency. These changes were probably aided by prevention programs utilizing both mass media and church-based, workplace-based, and other interpersonal communication activities. The main lesson emerging from these data which were published in the PloS medical journal online is that, unless prevention efforts can be made more effective, there will ultimately be no victory in the fight against HIV/AIDS. This lesson is for all countries worldwide.
giovedì 10 febbraio 2011
HIV, HPV and cervical cancer in developing countries
Both Cervical cancer and HIV infection are sexually transmitted diseases with no immediate visible symptoms. Cervical cancer originates from a sexually transmitted disease named Human Papilloma virus (HPV) which silently grows in the cervix and later develops to invasive cervical cancer. There is a growing evidence in the medical literature that a difference exists between HIV/AIDS positive and HIV negative women in the incidence and aggressiveness of cervical cancer, and this latter tumor is now regarded as an AIDS defining illness. This is particulary true in the low income developing world. Researchers suggest that as women are living longer due to access to specific anti-retroviral drugs, they are at an increased risk of contracting cervical cancer. While access to antiretroviral therapy is beginning to reduce AIDS mortality worldwide, gynaecologic oncologists warn that women being treated for AIDS could end up dying of cervical cancer unless they have access to appropriate screening and treatment. In fact, HIV positive women commonly show invasive cancer ten years earlier than women who are HIV negative. Moreover, the incidence of the precursor of cervical cancer, i.e. cervical intraepithelial neoplasia (CIN) is 4-5 times higher among HIV-infected than HIV-negative women and girls. In conclusion, there is a need for successful integration of cervical cancer and HIV/AIDS service especially in low income developing countries. Great efforts should be made to introduce HPV vaccination in young girls and to implement effective secondary prevention and early diagnosis of cervical cancer in HIV positive women.
domenica 6 febbraio 2011
breast cancer incidence in 2008 worldwide
 |
| Estimated age-standardised rates (World) per 100,000 |
Using the same source as in the previous post I am reporting the incidence of breast cancer worldwide in 2008.
“Breast cancer is by far the most frequent cancer among women with an estimated 1.38 million new cancer cases diagnosed in 2008 (23% of all cancers), and ranks second overall (10.9% of all cancers). It is now the most common cancer both in developed and developing regions with around 690 000 new cases estimated in each region (population ratio 1:4). Incidence rates vary from 19.3 per 100,000 women in Eastern Africa to 89.7 per 100,000 women in Western Europe, and are high (greater than 80 per 100,000) in developed regions of the world (except Japan) and low (less than 40 per 100,000) in most of the developing regions. The range of mortality rates is much less (approximately 6-19 per 100,000) because of the more favorable survival of breast cancer in (high-incidence) developed regions. As a result, breast cancer ranks as the fifth cause of death from cancer overall (458 000 deaths), but it is still the most frequent cause of cancer death in women in both developing (269 000 deaths, 12.7% of total) and developed regions, where the estimated 189 000 deaths is almost equal to the estimated number of deaths from lung cancer (188 000 deaths). “
It is also interesting to note that although the incidence of breast cancer in developing countries is significantly lower than in developed countries, mortality due to this tumor is much higher in the former as compared to the latter. As already pointed out in previous posts, this is due to the lack of efficient screening and early diagnosis of breast cancer in developing countries.
uterine cervical cancer incidence in 2008 worldwide
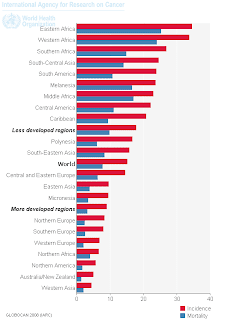 |
| Estimated age-standardised rates (World) per 100,000 |
Here are some some updated data on the incidence of cervical cancer worldwide according to the International agency for research on cancer (IARC). Cervical cancer is the third most common cancer in women, and the seventh overall, with an estimated 530 000 new cases in 2008. More than 85% of the global burden occurs in developing countries, where it accounts for 13% of all female cancers. High-risk regions are Eastern and Western Africa with age standardised incidence rate (ASR) greater then 30 per 100,000, Southern Africa (ASR 26.8 per 100,000), South-Central Asia (ASR 24.6 per 100,000), South America and Middle Africa (ASRs 23.9 and 23.0 per 100,000 respectively). Rates are lowest in Western Asia, Northern America and Australia/New Zealand (ASRs less than 6 per 100,00). Cervical cancer remains the most common cancer in women only in Eastern Africa, South-Central Asia and Melanesia. Overall, the mortality incidence ratio is 52%, and cervical cancer was responsible for 275 000 deaths in 2008, about 88% of which occurred in developing countries.
giovedì 3 febbraio 2011
africa needs a green revolution
Africa’s peasants are migrating to the cities in huge numbers because it is becoming increasingly difficult to survive on their farms. Meanwhile, very few are finding productive jobs in the cities and most are getting poorer. Africa’s dependance on concessionary food import is growing and these trends can have catastrophic consequences for the continent’s poor people. Current situation in Africa bears some striking similarities in Asia in the early 1960s. Faced with worsening food shortages and slow agricultural growth, Asian governments started spending 10-15% of their total budget on agriculture each year because they realised that rapid agricultural growth was a key step along the path to industrialisation. They invested on agricultural research, irrigation, rural roads and power. Many of these interventions were targeted to small farms, who enthusiastically adopted the new technologies and typically outperformed larger farms. These policies inspired a green revolution that helped transform Asia. Africa, in contrast, has failed to do the same. For over 40 years African governments have spent less than half the share spent in Asia, and little has been done for agricultural development. Africa has only exploited a fraction of its irrigation potential and the density of rural roads is very low. Farmers rely almost exclusively on rain-fed farming and face exceptionally high transport and marketing costs. Instead, yields could dramatically increase if farmers had access to improved technologies and markets and if goverments provided more supportive policies for agriculture. An African green revolution would generate many productive jobs in agriculture and provide a leg up out of poverty for many. This would help creating allied industries and lowering food prices, and, finally, would prevent migration of millions of peasants off the land. Two risks, however, should be taken into account: a) the spread of green revolution agriculture may affect both agricultural biodiversity and wild biodiversity; b) the consumption of the chemicals and pesticides used to kill pests by humans in some cases may be increasing the likelihood of cancer.
Click here to read more on the topic.
Click here to read more on the topic.
martedì 25 gennaio 2011
too early and too late cancer detection
In clinical practice, the suspicion of cancer leads to biopsy and biopsy generally requires surgical excision or removal of the lesion. As a matter of fact, sometimes the lesion turns to be benign (a cancer mimic) or premalignant (i.e. lacking the full features of malignancy) or, if malignant, to represent a very early step of the disease (and one cannot be sure that the tumor would have behaved as an aggressive disease if left untreated). These possible events lead to overdiagnosis of cancer which is responsible for unjustified mutilation, anxiety of the patient, and cost escalation. A paper published in the Journal of the National Cancer Institute in 2010 has stirred up another round of debate about this topic. To mitigate the ongoing problem of cancer overdiagnosis, the authors of the above paper suggest three possibilities: raising the threshold of labeling a test abnormal, waiting for the growth of a lesion over time before biopsying, and ignoring smaller abnormalities. In summary, we are realizing that it is better not to continue on the path where we are compelled to investigate and treat anything that resembles cancer.
This is what is happening in the high-income developed countries of the world where screening procedures are highly effective in the detection of early cancer and its mimics. The best examples are cancer of the uterine cervix, the breast, the lung, etc. The opposite is true, instead, in the low-income developing countries where the above malignancies are detected too late due to the lack of resources in screening and secondary prevention, and the chance of successful treatment are low or null. For example, it is estimated that over 1 million women worldwide currently have cervical cancer, most of whom (living in developing countries) have not been diagnosed, or have no access to treatment that could cure them or prolong their life. According to the World Health Organization, in 2005, almost 260 000 women died of the disease, nearly 95% of them in developing countries, making cervical cancer one of the gravest threats to women’s lives. In these areas, cervical cancer is the most common cancer in women and the leading cause of cancer death among women.
domenica 23 gennaio 2011
urbanisation and cancer in africa
Both in developed and low-income developing countries of the world more than half of humanity resides now in cities, and city dwellers make up more of the world population each year. Humanity is abandoning the countryside and soon more than 25 cities will have populations of 10 million or more. Rural areas depopulate because modern farming techniques require less labor and more technology. In developing countries more and more migrants each year are leaving marginal lands because little rain and poor soils keep agricultural productivity low. In fact, farming income cannot compete with economic opportunities in cities. A growing, affluent urban class thus drives demand in energy and consumer goods and is straining city infrastructure.
Since 1955 Africa has witnessed the most rapid urbanisation of all the continents, giving rise to cities that rival some of the greatest in the world in terms of size and population although sadly not infrastructure. By the year 2025, 54.0 percent of the African population will reside in urban areas. Some of these cities are Kano, Cape Town, Johannesburg, Abidjan (all with a population of more than 3 million), Khartoum (Pop 4.5 million), Kinshasa (Pop 6.0 million), and Lagos (Pop 10.9 million). The growth of Africa’s population is high while the rates of economic growth are low. As a consequence the growth of available health facilities in these huge metropolitan areas cannot parallel the rate of people urbanisation. In these huge cities “new” diseases such as cancer will reach unexpected rates in the near future due to population growth and ageing, combined with reduced mortality from infectious disease, and lack of primary and secondary preventive actions. Urbanisation in Africa is thus likely to play a major role in favoring the cancer epidemic the continent will be faced to in few years.
giovedì 20 gennaio 2011
the 5/80 cancer disequilibrium
In october 2010 an important article appeared in the prestigious British medical journal “The Lancet” on the topic of cancer in the developing countries. I am reporting some statements: “Once thought to be a problem almost exclusive to the developed world, cancer is now a leading cause of death and disability, and thus a health priority, in poor countries”… “Low-income and middle-income countries now bear a majority share of the burden of cancer, but their health systems are particularly ill prepared to meet this challenge. The rising proportion of cases in these countries is caused by population growth and ageing, combined with reduced mortality from infectious disease. In 1970, 15% of newly reported cancers were in developing countries, compared with 56% in 2008. By 2030, the proportion is expected to be 70%”... “Overall, case fatality from cancer (calculated as an approximation from the ratio of incidence to mortality in a specific year) is estimated to be 75% in countries of low income, 72% in countries of low-middle income, 64% in countries of high-middle income, and 46% in countries of high income”… “Without prevention, antitobacco campaigns, vaccination against human papillomavirus (HPV) and hepatitis B virus, and focus on early detection of some tumors, growth of the cancer burden in these countries could make treatment virtually unaffordable in the long term”... “Only a small proportion of global resources for cancer are spent in countries of low and middle income: several studies have reported an estimate of 5%. By contrast, these countries together account for almost 80% of the disability-adjusted life-years lost worldwide to cancer. Cancer is an underfunded health problem and an important cause of premature death in resource- poor settings, resulting in this staggering “5/80 cancer disequilibrium”.
giovedì 6 gennaio 2011
women's poverty, HIV infection, and cancer
Women bear a disproportionate burden of the world’s poverty. Statistics indicate that they are more likely than men to be poor and at risk of hunger. This is certainly due to the systematic discrimination they face in education, health care, employment and control of assets. According to some estimates, women represent 70 percent of the world’s poor.
More than 30 million people are today living with HIV and, globally, women now account for half of all infections. Yet women increasingly make up the majority in sub-Saharan Africa where young women ages 15–24 are up to six times more likely to be HIV-positive than young men of the same age.
Why does it happen? According to the UN women website, “gender inequality and violations of women’s rights make women and girls particularly susceptible, leaving them with less control than men over their bodies and their lives. Women and girls often have less information about HIV and fewer resources to take preventive measures. They face barriers to the negotiation of safer sex, including economic dependency and unequal power relations”.
What about women’s poverty and cancer incidence and mortality? I have already reported the higher incidence and the higher mortality of carcinoma of the cervix uteri in the developing world as compared to the high-income western world which is mainly due to the lack of primary or secondary prevention. Every day in Africa many women die of this totally preventable cancer which is related to human papilloma virus (HPV) infection. Most of them even ignored the disease they were suffering from. Other than the lack of medical care and health facilities in the countries they live in, gender inequality and violations of women’s rights do play a major role in this tragedy too.
domenica 2 gennaio 2011
malaria prevention is giving results
This is a new nice story about prevention. The U.N. health agency says the billions of dollars poured into the program have helped buy anti-malaria nets for almost 600 million people in sub-Saharan Africa, and this has contributed to a drop of over 50 percent in malaria cases in 11 African countries. There are 106 countries in the world where malaria remains endemic. Forty-three of these countries are in sub-Saharan Africa, which is the heartland of malaria in terms of the number of cases and deaths and the severity of illness. Investment in malaria control brings results. After so many years of deterioration and stagnation in the malaria situation, countries and their development partners are now on the offensive. In Africa, the distribution of insecticide-treated mosquito nets has increased dramatically.
In less than three years, the number of nets distributed has come close to the target of 350 million set in 2008. Also in Africa, the number of people protected by indoor residual spraying of insecticides rose 6-fold, from less than 13 million in 2005 to 75 million in 2009. In addition, worldwide, the number of ACT treatment courses procured (Artemisinin-based combination therapies, i.e. the most effective antimalarial drugs) increased from just over 11 million in 2005 to 158 million in 2009. Such massive increases in the delivery of interventions produced in eleven of Africa’s 43 endemic countries reductions of greater than 50% in either confirmed malaria cases or deaths over the past decade.
Malaria is an extremely complex disease that has been causing deaths and social disruption since the beginning of recorded human history. This is the first time in the history of these countries that reported new cases or deaths are decreasing.
Iscriviti a:
Commenti (Atom)
















